
Ontario Cancer Statistics 2020 Ch 5: Cancer Incidence Rates and Trends
Cancer incidence refers to the number of new cases of cancer diagnosed within a specific period. This chapter presents actual (non-projected) incidence rates and trends based on counts considered complete as of 2016 – the latest available year.
What's on this page
Over the past 3 decades, population aging and growth contributed far more to the number of new cancer cases than actual changes in cancer risk and cancer control practices (Figure 5.1).
In 2016, 81,409 new cases of cancer were diagnosed in Ontario, representing a 175% increase since 1981 (29,649 cases). Breaking down this 175% increase, approximately 94% is attributable to aging of the population, 67% to population growth and only 14% to changes in cancer risk and cancer control practices.
Probability of Developing Cancer
The probability of developing cancer refers to the average chance of being diagnosed with cancer over the course of a lifetime.
The probability of developing a specific type of cancer depends on many factors, including:
- the population’s characteristics (e.g., demographics)
- the prevalence of risk factors (e.g., age, family history of cancer, smoking, obesity)
- current life expectancy
In addition, the probabilities in this report reflect the average risks for the overall population and do not take into account personal risk factors. In other words, an individual’s risk may be higher or lower than the numbers reported here.
In Ontario, 1 in 2 people, or 45.3%, will develop cancer in their lifetime (not including non-melanoma skin cancer) (Table 5.1). The probability of developing cancer was nearly the same for both males and females, although it varies based on cancer type:
- Among males, the probability is highest for prostate (1 in 8), lung (1 in 12) and colorectal (1 in 14) cancers.
- Among females, the probability is highest for breast (1 in 8), lung (1 in 14) and colorectal (1 in 17) cancers.
| Cancer type | Both sexes | Males | Females | |||
|---|---|---|---|---|---|---|
| % | 1 in | % | 1 in | % | 1 in | |
| All cancers | 45.3% | 2 | 45.9% | 2 | 45.0% | 2 |
| Bladder | 1.9% | 52 | 3.0% | 33 | 1.0% | 103 |
| Brain | 0.7% | 138 | 0.8% | 122 | 0.6% | 156 |
| Breast (female) | 12.8% | 8 | n/a | n/a | 12.8% | 8 |
| Cervix | 0.6% | 157 | n/a | n/a | 0.6% | 157 |
| Colorectal | 6.5% | 15 | 7.0% | 14 | 6.0% | 17 |
| Esophagus | 0.6% | 168 | 0.9% | 113 | 0.3% | 310 |
| Hodgkin lymphoma | 0.2% | 421 | 0.3% | 397 | 0.2% | 448 |
| Kidney | 1.5% | 66 | 2.0% | 51 | 1.1% | 92 |
| Larynx | 0.3% | 341 | 0.5% | 198 | 0.1% | 1052 |
| Leukemia | 1.9% | 53 | 2.3% | 44 | 1.5% | 65 |
| Liver | 1.0% | 101 | 1.3% | 75 | 0.7% | 150 |
| Lung | 7.6% | 13 | 8.0% | 12 | 7.3% | 14 |
| Melanoma | 2.4% | 42 | 2.8% | 35 | 2.0% | 51 |
| Myeloma | 1.1% | 95 | 1.2% | 80 | 0.9% | 112 |
| Non-Hodgkin lymphoma | 3.0% | 33 | 3.5% | 29 | 2.7% | 38 |
| Oral cavity & pharynx | 1.3% | 79 | 1.8% | 57 | 0.8% | 123 |
| Ovary | 1.6% | 62 | n/a | n/a | 1.6% | 62 |
| Pancreas | 1.7% | 60 | 1.7% | 59 | 1.6% | 62 |
| Prostate | 11.9% | 8 | 11.9% | 8 | n/a | n/a |
| Stomach | 1.2% | 83 | 1.5% | 65 | 0.9% | 113 |
| Testis | 0.4% | 230 | 0.4% | 230 | n/a | n/a |
| Thyroid | 1.8% | 57 | 0.9% | 110 | 2.6% | 38 |
| Uterus | 3.4% | 30 | n/a | n/a | 3.4% | 30 |
Analysis by: Surveillance, Analytics and Informatics, Ontario Health (Cancer Care Ontario)
Data source: Ontario Cancer Registry (December 2018), Ontario Health (Cancer Care Ontario). Statistics Canada, Canadian Vital Statistics, Birth and Death Databases and population estimates (formerly CANSIM 102-0504)
Incidence by Sex and Cancer Type
In 2016, 81,409 new cases of cancer were diagnosed in Ontario, for an age-standardized incidence rate (ASIR) of 544.0 per 100,000 (Table 5.2).
| Cancer group | Cancer type | Both sexes | Males | Females | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| New cases | % of cases | ASIR | ASIR 95% CI | New cases | % of cases | ASIR | ASIR 95% CI | New cases | % of cases | ASIR | ASIR 95% CI | ||
| All | All cancers | 81,409 | 100% | 544.0 | 540.2 - 547.7 | 40,628 | 100% | 584.3 | 578.6 - 590.0 | 40,781 | 100% | 517.7 | 512.7 - 522.8 |
| Brain & nervous system | Brain and other nervous system - malignant | 1,105 | 1.4% | 7.6 | 7.1 - 8.0 | 620 | 1.5% | 8.9 | 8.3 - 9.7 | 485 | 1.2% | 6.4 | 5.8 - 7.0 |
| Glioblastoma | 580 | 0.7% | 3.9 | 3.6 - 4.2 | 332 | 0.8% | 4.7 | 4.2 - 5.3 | 248 | 0.6% | 3.2 | 2.8 - 3.6 | |
| Meninges - malignant | 13 | 0.0% | 0.1 | 0.0 - 0.1 | ** | ** | ** | ** | ** | ** | ** | ** | |
| Brain and other nervous system - non-malignant | 2,309 | 2.8% | 15.8 | 15.2 - 16.5 | 938 | 2.3% | 13.6 | 12.8 - 14.6 | 1,371 | 3.4% | 17.9 | 16.9 - 18.9 | |
| Meninges - non-malignant | 947 | 1.2% | 6.4 | 6.0 - 6.8 | 300 | 0.7% | 4.4 | 3.9 - 4.9 | 647 | 1.6% | 8.2 | 7.6 - 8.9 | |
| Pituitary, pineal and craniopharyngeal duct | 512 | 0.6% | 3.5 | 3.2 - 3.9 | 253 | 0.6% | 3.6 | 3.2 - 4.1 | 259 | 0.6% | 3.5 | 3.1 - 4.0 | |
| Breast & genital system | Breast (female) | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | 11,192 | 27.4% | 145.2 | 142.5 - 148.0 |
| Cervix | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | 600 | 1.5% | 8.3 | 7.6 - 9.0 | |
| Ovary | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | 1,243 | 3.0% | 16.1 | 15.3 - 17.1 | |
| Prostate | n/a | n/a | n/a | n/a | 8,414 | 20.7% | 118.0 | 115.5 - 120.5 | n/a | n/a | n/a | n/a | |
| Testis | n/a | n/a | n/a | n/a | 467 | 1.1% | 6.9 | 6.3 - 7.5 | n/a | n/a | n/a | n/a | |
| Uterus | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | 2,824 | 6.9% | 36.3 | 34.9 - 37.6 | |
| Uterus - endometrial | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | 2,577 | 6.3% | 33.1 | 31.8 - 34.4 | |
| Uterus - uterine sarcoma | n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a | 84 | 0.2% | 1.2 | 0.9 - 1.4 | |
| Digestive system | Colorectal | 8,525 | 10.5% | 56.6 | 55.4 - 57.8 | 4,706 | 11.6% | 68.0 | 66.0 - 69.9 | 3,819 | 9.4% | 46.6 | 45.1 - 48.1 |
| Colon excluding rectum | 5,840 | 7.2% | 38.5 | 37.6 - 39.5 | 3,069 | 7.6% | 44.5 | 42.9 - 46.1 | 2,771 | 6.8% | 33.4 | 32.2 - 34.7 | |
| Colon - left sided | 2,119 | 2.6% | 14.1 | 13.5 - 14.7 | 1,247 | 3.1% | 18.0 | 17.0 - 19.0 | 872 | 2.1% | 10.9 | 10.2 - 11.6 | |
| Colon - right sided | 3,268 | 4.0% | 21.4 | 20.7 - 22.2 | 1,604 | 3.9% | 23.3 | 22.1 - 24.4 | 1,664 | 4.1% | 19.8 | 18.8 - 20.8 | |
| Rectum and rectosigmoid junction | 2,663 | 3.3% | 17.9 | 17.2 - 18.6 | 1,631 | 4.0% | 23.4 | 22.3 - 24.6 | 1,032 | 2.5% | 13.0 | 12.2 - 13.8 | |
| Rectosigmoid junction | 599 | 0.7% | 4.0 | 3.7 - 4.3 | 355 | 0.9% | 5.1 | 4.6 - 5.7 | 244 | 0.6% | 3.0 | 2.6 - 3.4 | |
| Rectum | 2,064 | 2.5% | 13.9 | 13.3 - 14.5 | 1,276 | 3.1% | 18.3 | 17.3 - 19.3 | 788 | 1.9% | 10.0 | 9.3 - 10.8 | |
| Esophagus | 808 | 1.0% | 5.3 | 5.0 - 5.7 | 606 | 1.5% | 8.7 | 8.0 - 9.4 | 202 | 0.5% | 2.5 | 2.1 - 2.8 | |
| Esophagus - adenocarcinoma | 494 | 0.6% | 3.3 | 3.0 - 3.6 | 407 | 1.0% | 5.8 | 5.3 - 6.4 | 87 | 0.2% | 1.1 | 0.9 - 1.3 | |
| Esophagus - squamous cell carcinoma | 226 | 0.3% | 1.5 | 1.3 - 1.7 | 137 | 0.3% | 1.9 | 1.6 - 2.3 | 89 | 0.2% | 1.1 | 0.9 - 1.3 | |
| Liver | 1,270 | 1.6% | 8.4 | 7.9 - 8.9 | 889 | 2.2% | 12.7 | 11.9 - 13.5 | 381 | 0.9% | 4.6 | 4.1 - 5.1 | |
| Pancreas | 2,056 | 2.5% | 13.5 | 12.9 - 14.1 | 1,096 | 2.7% | 15.9 | 14.9 - 16.8 | 960 | 2.4% | 11.5 | 10.8 - 12.3 | |
| Stomach | 1,529 | 1.9% | 10.1 | 9.6 - 10.7 | 978 | 2.4% | 14.2 | 13.3 - 15.1 | 551 | 1.4% | 6.8 | 6.2 - 7.4 | |
| Head and neck | Larynx | 414 | 0.5% | 2.7 | 2.5 - 3.0 | 346 | 0.9% | 4.9 | 4.4 - 5.4 | 68 | 0.2% | 0.8 | 0.7 - 1.1 |
| Oral cavity & pharynx | 1,690 | 2.1% | 11.4 | 10.8 - 11.9 | 1,163 | 2.9% | 16.6 | 15.6 - 17.6 | 527 | 1.3% | 6.6 | 6.1 - 7.2 | |
| Lip and oral cavity | 776 | 1.0% | 5.2 | 4.8 - 5.6 | 450 | 1.1% | 6.5 | 5.9 - 7.1 | 326 | 0.8% | 4.0 | 3.6 - 4.5 | |
| Hypopharynx | 93 | 0.1% | 0.6 | 0.5 - 0.8 | 73 | 0.2% | 1.1 | 0.8 - 1.3 | 20 | 0.0% | 0.3 | 0.2 - 0.4 | |
| Nasopharynx | 128 | 0.2% | 0.9 | 0.8 - 1.1 | 95 | 0.2% | 1.4 | 1.1 - 1.7 | 33 | 0.1% | 0.5 | 0.3 - 0.6 | |
| Oropharynx | 629 | 0.8% | 4.2 | 3.9 - 4.6 | 503 | 1.2% | 7.1 | 6.5 - 7.7 | 126 | 0.3% | 1.6 | 1.3 - 1.9 | |
| Thyroid | 3,013 | 3.7% | 21.4 | 20.7 - 22.2 | 780 | 1.9% | 11.3 | 10.5 - 12.1 | 2,233 | 5.5% | 31.2 | 29.9 - 32.5 | |
| Thyroid - anaplastic | 15 | 0.0% | 0.1 | 0.1 - 0.2 | 8 | 0.0% | 0.1 | 0.1 - 0.2 | 7 | 0.0% | 0.1 | 0.0 - 0.2 | |
| Thyroid - follicular | 96 | 0.1% | 0.7 | 0.5 - 0.8 | 22 | 0.1% | 0.3 | 0.2 - 0.5 | 74 | 0.2% | 1.0 | 0.8 - 1.3 | |
| Thyroid - medullary | 39 | 0.0% | 0.3 | 0.2 - 0.4 | 16 | 0.0% | 0.2 | 0.1 - 0.4 | 23 | 0.1% | 0.3 | 0.2 - 0.5 | |
| Thyroid - papillary | 2,790 | 3.4% | 19.9 | 19.2 - 20.6 | 708 | 1.7% | 10.3 | 9.5 - 11.1 | 2,082 | 5.1% | 29.2 | 27.9 - 30.4 | |
| Hematological | Leukemia | 2,396 | 2.9% | 16.1 | 15.4 - 16.7 | 1,447 | 3.6% | 21.0 | 20.0 - 22.2 | 949 | 2.3% | 11.9 | 11.2 - 12.7 |
| Acute lymphocytic leukemia | 205 | 0.3% | 1.5 | 1.3 - 1.7 | 123 | 0.3% | 1.8 | 1.5 - 2.1 | 82 | 0.2% | 1.2 | 0.9 - 1.5 | |
| Acute monocytic leukemia | 81 | 0.1% | 0.6 | 0.4 - 0.7 | 52 | 0.1% | 0.8 | 0.6 - 1.0 | 29 | 0.1% | 0.4 | 0.3 - 0.5 | |
| Acute myeloid leukemia | 651 | 0.8% | 4.4 | 4.0 - 4.7 | 372 | 0.9% | 5.5 | 4.9 - 6.1 | 279 | 0.7% | 3.5 | 3.1 - 3.9 | |
| Chronic lymphocytic leukemia | 811 | 1.0% | 5.3 | 5.0 - 5.7 | 512 | 1.3% | 7.3 | 6.7 - 8.0 | 299 | 0.7% | 3.6 | 3.2 - 4.1 | |
| Chronic myeloid leukemia | 350 | 0.4% | 2.4 | 2.1 - 2.6 | 214 | 0.5% | 3.1 | 2.7 - 3.6 | 136 | 0.3% | 1.7 | 1.4 - 2.0 | |
| Lymphoma | 4,772 | 5.9% | 32.2 | 31.3 - 33.1 | 2,622 | 6.5% | 38.1 | 36.6 - 39.6 | 2,150 | 5.3% | 27.2 | 26.1 - 28.4 | |
| Hodgkin lymphoma | 412 | 0.5% | 2.9 | 2.7 - 3.2 | 222 | 0.5% | 3.2 | 2.8 - 3.7 | 190 | 0.5% | 2.7 | 2.3 - 3.1 | |
| Non-Hodgkin lymphoma | 4,360 | 5.4% | 29.2 | 28.4 - 30.1 | 2,400 | 5.9% | 34.8 | 33.4 - 36.3 | 1,960 | 4.8% | 24.6 | 23.5 - 25.7 | |
| Non-Hodgkin lymphoma - extranodal | 2,319 | 2.8% | 15.5 | 14.9 - 16.2 | 1,276 | 3.1% | 18.6 | 17.5 - 19.6 | 1,043 | 2.6% | 13.0 | 12.2 - 13.8 | |
| Non-Hodgkin lymphoma - nodal | 2,041 | 2.5% | 13.7 | 13.1 - 14.3 | 1,124 | 2.8% | 16.3 | 15.3 - 17.3 | 917 | 2.2% | 11.5 | 10.8 - 12.3 | |
| Myeloma | 1,387 | 1.7% | 9.1 | 8.7 - 9.6 | 762 | 1.9% | 11.1 | 10.3 - 11.9 | 625 | 1.5% | 7.6 | 7.0 - 8.3 | |
| Melanoma | Melanoma of the skin | 3,851 | 4.7% | 25.9 | 25.0 - 26.7 | 2,230 | 5.5% | 32.5 | 31.1 - 33.9 | 1,621 | 4.0% | 20.8 | 19.8 - 21.9 |
| Melanoma (non-cutaneous) | 191 | 0.2% | 1.3 | 1.1 - 1.5 | 93 | 0.2% | 1.3 | 1.1 - 1.6 | 98 | 0.2% | 1.3 | 1.0 - 1.5 | |
| Melanoma - mucosal | 44 | 0.1% | 0.3 | 0.2 - 0.4 | 14 | 0.0% | 0.2 | 0.1 - 0.3 | 30 | 0.1% | 0.4 | 0.2 - 0.5 | |
| Melanoma - ocular | 147 | 0.2% | 1.0 | 0.8 - 1.2 | 79 | 0.2% | 1.1 | 0.9 - 1.4 | 68 | 0.2% | 0.9 | 0.7 - 1.1 | |
| Thoracic system | Lung | 9,958 | 12.2% | 65.1 | 63.8 - 66.4 | 4,922 | 12.1% | 70.8 | 68.8 - 72.8 | 5,036 | 12.3% | 61.2 | 59.5 - 62.9 |
| Lung - adenocarcinoma | 4,308 | 5.3% | 28.3 | 27.5 - 29.2 | 1,883 | 4.6% | 26.9 | 25.7 - 28.1 | 2,425 | 5.9% | 29.9 | 28.7 - 31.1 | |
| Lung - large cell | 130 | 0.2% | 0.9 | 0.7 - 1.0 | 67 | 0.2% | 0.9 | 0.7 - 1.2 | 63 | 0.2% | 0.8 | 0.6 - 1.0 | |
| Lung - small cell | 943 | 1.2% | 6.2 | 5.8 - 6.6 | 495 | 1.2% | 7.0 | 6.4 - 7.6 | 448 | 1.1% | 5.5 | 5.0 - 6.1 | |
| Lung - squamous cell | 1,688 | 2.1% | 10.9 | 10.4 - 11.5 | 1,063 | 2.6% | 15.2 | 14.3 - 16.1 | 625 | 1.5% | 7.5 | 6.9 - 8.1 | |
| Urinary system | Bladder | 4,237 | 5.2% | 27.7 | 26.9 - 28.6 | 3,195 | 7.9% | 46.7 | 45.0 - 48.3 | 1,042 | 2.6% | 12.5 | 11.8 - 13.3 |
| Kidney | 2,438 | 3.0% | 16.5 | 15.8 - 17.2 | 1,590 | 3.9% | 22.7 | 21.6 - 23.9 | 848 | 2.1% | 10.9 | 10.1 - 11.6 | |
Abbreviations: ASIR means age-standardized incidence rate; CI means confidence interval.
Notes:
- Rates are per 100,000 and are age-standardized to the 2011 Canadian population.
- Only selected subsites and histological subtypes of major cancers are shown. As a result, counts for these may not sum to the total for the cancer type.
Analysis by: Surveillance, Analytics and Informatics, Ontario Health (Cancer Care Ontario)
Data source: Ontario Cancer Registry (December 2018), Ontario Health (Cancer Care Ontario)
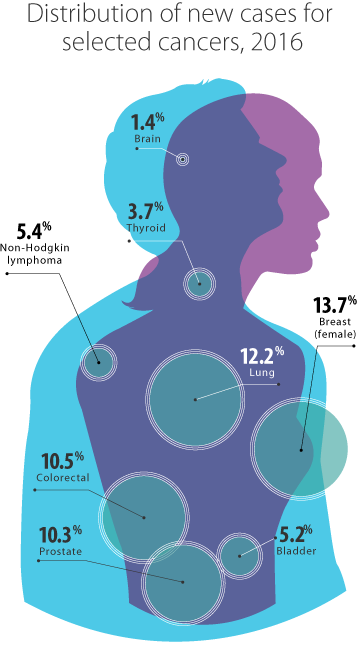
The 4 most commonly diagnosed cancers (lung, colorectal, breast and prostate) were responsible for almost 50% of all new cancer cases in 2016. By sex, lung, colorectal and prostate cancers accounted for 44% new cases among males, while lung, breast and colorectal cancers accounted for 49% of new cases among females (Figure 5.2).
Non-melanoma skin cancers represent the most common type of cancer in most jurisdictions, but they are not included in this report because Ontario does not routinely collect data about them. Other countries have reported an increasing trend in non-melanoma skin cancers.[1-3]
In 2016, the highest ASIRs for cancers occurring in both sexes were lung (65.1 per 100,000), colorectal (56.6 per 100,000) and lymphoma (32.2 per 100,000).
The ASIR for all cancers combined was significantly higher in males (584.3 per 100,000) than in females (517.7 per 100,000) (Table 5.2).
- In males, the most commonly diagnosed cancers were prostate (8,414, or 20.7% of all new male cases), lung (4,922, or 12.1%) and colorectal (4,706, or 11.6%).
- In females, the leading cancer types were breast (11,192, or 27.4% of all new female cases), lung (5,036, or 12.3%) and colorectal (3,819, or 9.4%).
The greatest difference in incidence between males and females was for the following cancers: laryngeal, bladder, esophageal, liver and intrahepatic bile duct, oral cavity and pharynx, stomach and kidney. Notably, the risk of each of these cancer types is associated with the use of either tobacco or alcohol,[4,5] and in Ontario, tobacco and alcohol use are more prevalent among men.[6]
- Laryngeal cancer: The male rate was over 6 times the female rate. Smokers are 7 times more likely to develop laryngeal cancers,[7] while heavy alcohol use more than doubles the risk.[4]
- Bladder cancer: The male rate was nearly 4 times the female rate. One of the main risk factors for bladder cancer is smoking, with smokers being 2 to 3 times more likely to develop bladder cancer than non-smokers.[8,9]
- Esophageal cancer: The overall male rate was more than 3 times the female rate, with the rate of adenocarcinoma of the esophagus more than 5 times greater in males than in females. Smoking more than doubles the risk of esophageal cancer.[7] Alcohol use and obesity — also more common in males — are other risk factors for esophageal cancer.[10]
- Liver cancer: The male rate was nearly 3 times greater than the female rate. Tobacco and alcohol use are both linked to increased risk of liver cancer.[4] Chronic viral hepatitis is another important risk factor for liver cancer.[11]
- Stomach cancer: The male rate was double the female rate. Heavy alcohol use is associated with a 20% increase in risk of stomach cancer. [4]
- Oral cavity and pharynx cancer: The male rate was more than twice the female rate, with the rate of oropharynx cancers in males over 4 times the female rate. Tobacco and alcohol use are important risk factors for oral cavity and pharynx cancer.[12] Alcohol use increases the risk by more than 5 times.[4]
- Kidney cancer: The male rate was double the female rate. Heavy alcohol use is associated with increased risk of kidney cancer.[4]
The incidence rate was higher in males than females for almost all cancers. An exception was thyroid cancer, for which the ASIR for females was 31.2 per 100,000 compared with just 11.3 per 100,000 in males. A number of possible reasons for the higher incidence of thyroid cancer in females have been proposed, including:
- a greater likelihood of diagnostic investigation among females because they are more likely to have thyroid disease,[13] as well as a greater tendency to seek medical attention and participate more actively in medical visits[14-16]
- the biological differences that exist in the hormone levels of males and females (such as thyroid stimulated hormone and sex steroids)[17-19]
While the incidence of less aggressive types of thyroid cancer, such as papillary carcinoma, is higher for females than males (Table 5.2), the rate of more aggressive types (such as anaplastic and medullary thyroid cancers) are generally similar between the sexes. The same is seen in other jurisdictions.[13,20] The result is similar for thyroid mortality rates between the sexes (see Chapter 6: Cancer Mortality Rates and Trends).
The incidence rates of non-malignant tumours of the brain and nervous system as well as lung adenocarcinoma were higher in females than males. Although the higher rate of non-malignant brain tumours in females also has been seen in many other jurisdictions,[21-24] the reason for these sex differences is not clear.
Incidence by Age
Between 2014 and 2016, the median age at cancer diagnosis was 67 years for both males and females (Table 5.3). The median age at diagnosis varied by cancer type. Of the 23 cancer types, cancers with the lowest median age (all under age 50 years) were testis, Hodgkin lymphoma and cervix. However, these cancer types are rare in children 0 to 14 years of age.
Childhood cancer types are unique. The childhood cancer types with the lowest median age at diagnosis include neuroblastoma, retinoblastoma and hepatic tumours. In addition, neuroblastoma, leukemias and central nervous system tumours are the most common types of cancer in children under 1 year of age.
For details about childhood cancer incidence, see Spotlight: Childhood Cancer Incidence, Table S1 or visit the POGO Surveillance Report.
With the exception of thyroid cancer, the median ages for all other cancer types were above age 60.
| Cancer type | Age (years) | ||
|---|---|---|---|
| Both sexes | Males | Females | |
| All cancers | 67 | 68 | 66 |
| Bladder | 73 | 73 | 73 |
| Brain | 61 | 60 | 62 |
| Breast (female) | 63 | n/a | 63 |
| Cervix | 49 | n/a | 49 |
| Colorectal | 70 | 69 | 72 |
| Esophagus | 69 | 68 | 72 |
| Hodgkin lymphoma | 38 | 37.5 | 38 |
| Kidney | 64 | 64 | 65 |
| Larynx | 68 | 68 | 69 |
| Leukemia | 68 | 68 | 68 |
| Liver | 68 | 67 | 72 |
| Lung | 71 | 72 | 71 |
| Melanoma | 66 | 68 | 63 |
| Myeloma | 71 | 71 | 72 |
| Non-Hodgkin lymphoma | 68 | 67 | 69 |
| Oral cavity & pharynx | 64 | 63 | 66 |
| Ovary | 63 | n/a | 63 |
| Pancreas | 71 | 70 | 74 |
| Prostate | 68 | 68 | n/a |
| Stomach | 70 | 70 | 70 |
| Testis | 34 | 34 | n/a |
| Thyroid | 51 | 55 | 50 |
| Uterus | 64 | n/a | 64 |
Analysis by: Surveillance, Analytics and Informatics, Ontario Health (Cancer Care Ontario)
Data source: Ontario Cancer Registry (December 2018), Ontario Health (Cancer Care Ontario)
In 2016, more than half of all newly diagnosed cancer cases were in people ages 60 to 79 (Table 5.4). The distribution of cancer types by age group varied widely.
| Cancer group | Cancer type | Ages 0 - 39 years | Ages 40 - 59 years | Ages 60 - 79 years | 80 years or older | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| New cases | Age-specific rate | 95 % CI | New cases | Age-specific rate | 95 % CI | New cases | Age-specific rate | 95 % CI | New cases | Age-specific rate | 95 % CI | ||
| All | All cancers | 4,091 | 59.6 | 57.7 - 61.4 | 19,496 | 493.1 | 486.2 - 500.1 | 42,396 | 1,662.6 | 1,646.8 - 1,678.5 | 15,426 | 2,559.7 | 2,519.4 - 2,600.4 |
| Brain & nervous system | Brain and other nervous system - Malignant* | 210 | 3.1 | 2.7 - 3.5 | 308 | 7.8 | 6.9 - 8.7 | 441 | 17.3 | 15.7 - 19.0 | 146 | 24.2 | 20.5 - 28.5 |
| Glioblastoma | 34 | 0.5 | 0.3 - 0.7 | 173 | 4.4 | 3.7 - 5.1 | 307 | 12.0 | 10.7 - 13.5 | 66 | 11.0 | 8.5 - 13.9 | |
| Meninges - malignant | ** | ** | ** | ** | ** | ** | 7 | 0.3 | 0.1 - 0.6 | ** | ** | ** | |
| Brain and other nervous system - Non-malignant | 372 | 5.4 | 4.9 - 6.0 | 742 | 18.8 | 17.4 - 20.2 | 824 | 32.3 | 30.1 - 34.6 | 371 | 61.6 | 55.5 - 68.2 | |
| Meninges - non-malignant | 55 | 0.8 | 0.6 - 1.0 | 298 | 7.5 | 6.7 - 8.4 | 395 | 15.5 | 14.0 - 17.1 | 199 | 33.0 | 28.6 - 37.9 | |
| Pituitary, pineal and craniopharyngeal duct | 127 | 1.8 | 1.5 - 2.2 | 177 | 4.5 | 3.8 - 5.2 | 170 | 6.7 | 5.7 - 7.7 | 38 | 6.3 | 4.5 - 8.7 | |
| Breast & genital system | Breast (female) | 463 | 13.6 | 12.4 - 14.9 | 4,103 | 205.4 | 199.1 - 211.8 | 5,143 | 384.5 | 374.1 - 395.2 | 1,483 | 404.7 | 384.4 - 425.9 |
| Cervix | 176 | 5.2 | 4.4 - 6.0 | 251 | 12.6 | 11.1 - 14.2 | 135 | 10.1 | 8.5 - 11.9 | 38 | 10.4 | 7.3 - 14.2 | |
| Ovary | 87 | 2.6 | 2.0 - 3.2 | 423 | 21.2 | 19.2 - 23.3 | 555 | 41.5 | 38.1 - 45.1 | 178 | 48.6 | 41.7 - 56.3 | |
| Prostate | ** | ** | ** | 1,425† | 72.9 | 69.1 - 76.7 | 5,845 | 482.1 | 469.8 - 494.6 | 1,140 | 482.5 | 454.9 - 511.4 | |
| Testis | 300 | 8.7 | 7.7 - 9.7 | 133 | 6.8 | 5.7 - 8.1 | 26 | 2.1 | 1.4 - 3.1 | 8 | 3.4 | 1.5 - 6.7 | |
| Uterus | 62 | 1.8 | 1.4 - 2.3 | 901 | 45.1 | 42.2 - 48.1 | 1,600 | 119.6 | 113.8 - 125.6 | 261 | 71.2 | 62.9 - 80.4 | |
| Uterus - endometrial | 46 | 1.4 | 1.0 - 1.8 | 820 | 41.0 | 38.3 - 44.0 | 1,501 | 112.2 | 106.6 - 118.0 | 210 | 57.3 | 49.8 - 65.6 | |
| Uterus - uterine sarcoma | ** | ** | ** | 50 | 2.5 | 1.9 - 3.3 | 25 | 1.9 | 1.2 - 2.8 | ** | ** | ** | |
| Digestive system | Colorectal | 168 | 2.4 | 2.1 - 2.8 | 1,856 | 46.9 | 44.8 - 49.1 | 4,353 | 170.7 | 165.7 - 175.9 | 2,148 | 356.4 | 341.5 - 371.8 |
| Colon excluding rectum* | 99 | 1.4 | 1.2 - 1.8 | 1,049 | 26.5 | 24.9 - 28.2 | 3,035 | 119.0 | 114.8 - 123.3 | 1,657 | 274.9 | 261.9 - 288.5 | |
| Colon - left sided | 55 | 0.8 | 0.6 - 1.0 | 506 | 12.8 | 11.7 - 14.0 | 1,114 | 43.7 | 41.2 - 46.3 | 444 | 73.7 | 67.0 - 80.9 | |
| Colon - right sided* | 36 | 0.5 | 0.4 - 0.7 | 451 | 11.4 | 10.4 - 12.5 | 1,756 | 68.9 | 65.7 - 72.2 | 1,025 | 170.1 | 159.8 - 180.8 | |
| Rectum and rectosigmoid junction | 69 | 1.0 | 0.8 - 1.3 | 806 | 20.4 | 19.0 - 21.8 | 1,316 | 51.6 | 48.9 - 54.5 | 472 | 78.3 | 71.4 - 85.7 | |
| Rectosigmoid junction | 13 | 0.2 | 0.1 - 0.3 | 166 | 4.2 | 3.6 - 4.9 | 286 | 11.2 | 10.0 - 12.6 | 134 | 22.2 | 18.6 - 26.3 | |
| Rectum | 56 | 0.8 | 0.6 - 1.1 | 640 | 16.2 | 15.0 - 17.5 | 1,030 | 40.4 | 38.0 - 42.9 | 338 | 56.1 | 50.3 - 62.4 | |
| Esophagus | 8 | 0.1 | 0.1 - 0.2 | 160 | 4.0 | 3.4 - 4.7 | 484 | 19.0 | 17.3 - 20.7 | 156 | 25.9 | 22.0 - 30.3 | |
| Esophagus - adenocarcinoma | ** | ** | ** | 110† | 2.8 | 2.3 - 3.4 | 293 | 11.5 | 10.2 - 12.9 | 85 | 14.1 | 11.3 - 17.4 | |
| Esophagus - squamous cell carcinoma | ** | ** | ** | 40† | 1.0 | 0.7 - 1.4 | 145 | 5.7 | 4.8 - 6.7 | 39 | 6.5 | 4.6 - 8.8 | |
| Liver | 22 | 0.3 | 0.2 - 0.5 | 242 | 6.1 | 5.4 - 6.9 | 732 | 28.7 | 26.7 - 30.9 | 274 | 45.5 | 40.2 - 51.2 | |
| Pancreas | 26 | 0.4 | 0.2 - 0.6 | 358 | 9.1 | 8.1 - 10.0 | 1,101 | 43.2 | 40.7 - 45.8 | 571 | 94.7 | 87.1 - 102.8 | |
| Stomach | 34 | 0.5 | 0.3 - 0.7 | 320 | 8.1 | 7.2 - 9.0 | 808 | 31.7 | 29.5 - 33.9 | 367 | 60.9 | 54.8 - 67.5 | |
| Head and neck | Larynx | ** | ** | ** | 80† | 2 | 1.6 - 2.5 | 276 | 10.8 | 9.6 - 12.2 | 55 | 9.1 | 6.9 - 11.9 |
| Oral cavity & pharynx | 40 | 0.6 | 0.4 - 0.8 | 535 | 13.5 | 12.4 - 14.7 | 885 | 34.7 | 32.5 - 37.1 | 230 | 38.2 | 33.4 - 43.4 | |
| Hypopharynx | ** | ** | ** | 20 | 0.5 | 0.3 - 0.8 | 60 | 2.4 | 1.8 - 3.0 | 10† | 1.7 | 0.8 - 3.1 | |
| Lip and oral cavity | 25 | 0.4 | 0.2 - 0.5 | 200 | 5.1 | 4.4 - 5.8 | 389 | 15.3 | 13.8 - 16.8 | 162 | 26.9 | 22.9 - 31.4 | |
| Nasopharynx | 11 | 0.2 | 0.1 - 0.3 | 71 | 1.8 | 1.4 - 2.3 | 39 | 1.5 | 1.1 - 2.1 | 7 | 1.2 | 0.5 - 2.4 | |
| Oropharynx | ** | ** | ** | 230† | 5.8 | 5.1 - 6.6 | 361 | 14.2 | 12.7 - 15.7 | 36 | 6.0 | 4.2 - 8.3 | |
| Thyroid | 737 | 10.7 | 10.0 - 11.5 | 1,363 | 34.5 | 32.7 - 36.4 | 832 | 32.6 | 30.4 - 34.9 | 81 | 13.4 | 10.7 - 16.7 | |
| Thyroid - anaplastic | ** | ** | ** | ** | ** | ** | 9 | 0.4 | 0.2 - 0.7 | ** | ** | ** | |
| Thyroid - follicular | 30 | 0.4 | 0.3 - 0.6 | 29 | 0.7 | 0.5 - 1.1 | 30† | 1.2 | 0.8 - 1.7 | ** | ** | ** | |
| Thyroid - medullary | 10† | 0.1 | 0.1 - 0.3 | 15 | 0.4 | 0.2 - 0.6 | 15 | 0.6 | 0.3 - 1.0 | ** | ** | ** | |
| Thyroid - papillary | 691 | 10.1 | 9.3 - 10.8 | 1,293 | 32.7 | 30.9 - 34.5 | 744 | 29.2 | 27.1 - 31.4 | 62 | 10.3 | 7.9 - 13.2 | |
| Hematological | Leukemia* | 265 | 3.9 | 3.4 - 4.4 | 470 | 11.9 | 10.8 - 13.0 | 1,138 | 44.6 | 42.1 - 47.3 | 523 | 86.8 | 79.5 - 94.5 |
| Acute lymphocytic leukemia | 127 | 1.8 | 1.5 - 2.2 | 34 | 0.9 | 0.6 - 1.2 | 32 | 1.3 | 0.9 - 1.8 | 12 | 2.0 | 1.0 - 3.5 | |
| Acute monocytic leukemia* | 11 | 0.2 | 0.1 - 0.3 | 18 | 0.5 | 0.3 - 0.7 | 40 | 1.6 | 1.1 - 2.1 | 12 | 2.0 | 1.0 - 3.5 | |
| Acute myeloid leukemia* | 65 | 0.9 | 0.7 - 1.2 | 126 | 3.2 | 2.7 - 3.8 | 307 | 12.0 | 10.7 - 13.5 | 153 | 25.4 | 21.5 - 29.7 | |
| Chronic lymphocytic leukemia | 7 | 0.1 | 0.0 - 0.2 | 149 | 3.8 | 3.2 - 4.4 | 489 | 19.2 | 17.5 - 21.0 | 166 | 27.5 | 23.5 - 32.1 | |
| Chronic myeloid leukemia* | 38 | 0.6 | 0.4 - 0.8 | 75 | 1.9 | 1.5 - 2.4 | 148 | 5.8 | 4.9 - 6.8 | 89 | 14.8 | 11.9 - 18.2 | |
| Lymphoma* | 499 | 7.3 | 6.6 - 7.9 | 1,090 | 27.6 | 26.0 - 29.3 | 2,255 | 88.4 | 84.8 - 92.2 | 928 | 154.0 | 144.2 - 164.2 | |
| Hodgkin lymphoma | 221 | 3.2 | 2.8 - 3.7 | 98 | 2.5 | 2.0 - 3.0 | 70 | 2.7 | 2.1 - 3.5 | 23 | 3.8 | 2.4 - 5.7 | |
| Non-hodgkin lymphoma* | 278 | 4.0 | 3.6 - 4.6 | 992 | 25.1 | 23.6 - 26.7 | 2,185 | 85.7 | 82.1 - 89.4 | 905 | 150.2 | 140.5 - 160.3 | |
| NHL - extranodal* | 169 | 2.5 | 2.1 - 2.9 | 497 | 12.6 | 11.5 - 13.7 | 1,118 | 43.8 | 41.3 - 46.5 | 535 | 88.8 | 81.4 - 96.6 | |
| NHL - nodal | 109 | 1.6 | 1.3 - 1.9 | 495 | 12.5 | 11.4 - 13.7 | 1,067 | 41.8 | 39.4 - 44.4 | 370 | 61.4 | 55.3 - 68.0 | |
| Myeloma | 11 | 0.2 | 0.1 - 0.3 | 243 | 6.1 | 5.4 - 7.0 | 757 | 29.7 | 27.6 - 31.9 | 376 | 62.4 | 56.2 - 69.0 | |
| Melanoma | Melanoma of the skin* | 254 | 3.7 | 3.3 - 4.2 | 1,017 | 25.7 | 24.2 - 27.4 | 1,762 | 69.1 | 65.9 - 72.4 | 818 | 135.7 | 126.6 - 145.4 |
| Melanoma (non-cutaneous) | 14 | 0.2 | 0.1 - 0.3 | 53 | 1.3 | 1.0 - 1.8 | 96 | 3.8 | 3.0 - 4.6 | 28 | 4.6 | 3.1 - 6.7 | |
| Melanoma - mucosal | ** | ** | ** | 10† | 0.3 | 0.1 - 0.5 | 24 | 0.9 | 0.6 - 1.4 | 11 | 1.8 | 0.9 - 3.3 | |
| Melanoma - ocular | 15† | 0.2 | 0.1 - 0.4 | 45 | 1.1 | 0.8 - 1.5 | 72 | 2.8 | 2.2 - 3.6 | 17 | 2.8 | 1.6 - 4.5 | |
| Thoracic system | Lung | 46 | 0.7 | 0.5 - 0.9 | 1,404 | 35.5 | 33.7 - 37.4 | 6,231 | 244.4 | 238.3 - 250.5 | 2,277 | 377.8 | 362.5 - 393.7 |
| Lung - adenocarcinoma | 19 | 0.3 | 0.2 - 0.4 | 727 | 18.4 | 17.1 - 19.8 | 2,781 | 109.1 | 105.0 - 113.2 | 781 | 129.6 | 120.7 - 139.0 | |
| Lung - large cell | ** | ** | ** | 20† | 0.5 | 0.3 - 0.8 | 94 | 3.7 | 3.0 - 4.5 | 16 | 2.7 | 1.5 - 4.3 | |
| Lung - small cell | ** | ** | ** | 160† | 4.0 | 3.4 - 4.7 | 650 | 25.5 | 23.6 - 27.5 | 132 | 21.9 | 18.3 - 26.0 | |
| Lung - squamous cell | ** | ** | ** | 140† | 3.6 | 3.0 - 4.2 | 1,169 | 45.8 | 43.3 - 48.5 | 377 | 62.6 | 56.4 - 69.2 | |
| Urinary system | Bladder | 37 | 0.5 | 0.4 - 0.7 | 520 | 13.2 | 12.0 - 14.3 | 2,436 | 95.5 | 91.8 - 99.4 | 1,244 | 206.4 | 195.1 - 218.2 |
| Kidney | 111 | 1.6 | 1.3 - 1.9 | 775 | 19.6 | 18.3 - 21.1 | 1,267 | 49.7 | 47.4 - 52.9 | 285 | 47.3 | 42.9 - 54.2 | |
Abbreviation: CI means confidence interval.
Symbols:
- *Significant increasing trend in age-specific rate with increasing age.
- **Suppressed due to small case count (less than 6).
- †Count has been rounded to ensure confidentiality; associated rate and confidence interval have been adjusted to reflect rounded count.
Notes:
- Rates are per 100,000.
- Excludes cases with no age information.
- Only selected subsites and histological subtypes of major cancers are shown. As a result, counts for these may not sum to the total for the cancer type.
Analysis by: Surveillance, Analytics and Informatics, Ontario Health (Cancer Care Ontario)
Data source: Ontario Cancer Registry (December 2018), Ontario Health (Cancer Care Ontario)
Ages 0 to 39 years
Five percent of all new cases occurred in people under age 40, with female breast and thyroid being the leading cancers.
The under-40 age group also accounted for the majority of new cases of Hodgkin lymphoma and testicular cancer, at 53.6% and 64.2%, respectively.
In 2016, about 0.5% of all new cancers occurred in children 0 to 14 years of age. Childhood cancer types are unique. The most common types are leukemias (32.5%), central nervous system tumours (23.7%) and lymphomas (12.8%) (see Spotlight: Childhood Cancer Incidence, Table S1).
For details about childhood cancer incidence, visit the POGO Surveillance Report.
Spotlight: Childhood Cancer Incidence
| Types of cancer/tumour (ICCC diagnosis group) | N | % | Age-specific incidence rate | ASIR | ASIR 95% CI |
|---|---|---|---|---|---|
| All cancers combined | 2,021 | 100.0% | 184.07 | 185.28 | 174.37 - 196.87 |
| I. Leukemias, myeloproliferative diseases, and myelodysplastic diseases | 656 | 32.5% | 59.75 | 60.25 | 57.45 - 63.19 |
| II. Lymphomas and reticuloendothelial neoplasms | 258 | 12.8% | 23.50 | 23.41 | 21.69 - 25.27 |
| III. CNS and miscellaneous intracranial and intraspinal neoplasms | 478 | 23.7% | 43.53 | 43.58 | 41.21 - 46.09 |
| IV. Neuroblastoma and other peripheral nervous system tumours | 137 | 6.8% | 13.39 | 13.76 | 12.41 - 15.26 |
| V. Retinoblastoma | 46 | 2.3% | 10.62 | 10.69 | 8.95 - 12.76 |
| VI. Renal tumours | 82 | 4.1% | 9.39 | 9.53 | 8.34 - 10.90 |
| VII. Hepatic tumours | 27 | 1.3% | 5.35 | 5.43 | 4.31 - 6.85 |
| VIII. Malignant bone tumours | 75 | 3.7% | 7.86 | 7.84 | 6.81 - 9.04 |
| IX. Soft tissue and other extraosseous sarcomas | 129 | 6.4% | 11.75 | 11.82 | 10.61 - 13.16 |
| X. Germ cell tumours, trophoblastic tumours, and neoplasms of gonads | 64 | 3.2% | 5.83 | 5.90 | 5.06 - 6.87 |
| XI. & XII. Other and unspecified malignant neoplasms | 69 | 3.4% | 6.28 | 6.30 | 5.43 - 7.30 |
Abbreviations: ASIR means age-standardized incidence rate; CI means confidence interval; CNS means central nervous system; ICCC means International Classification of Childhood Cancer
Notes:
- Rates are per 1,000,000.
- The POGONIS database classifies childhood cancer according to the International Classification of Childhood Cancer, third edition, which has 12 main diagnostic groups.
- Childhood cancer incidence is reported over 5-year period due to variations in annual incidence and potential for small cell disclosure.
Analysis by: Health Analytics, Pediatric Oncology Group of Ontario (POGO)
Data source: Pediatric Oncology Group of Ontario Networked Information System (POGONIS, October 16, 2019), POGO
Ages 40 to 59 years
Of all new cases, 23.9% occurred in people 40 to 59 years of age, with colorectal and female breast being the leading cancers.
Nearly half of all new cases of thyroid cancer occurred in people ages 40 to 59, and 41.8% of new cervical cancer cases occurred in females in this age group.
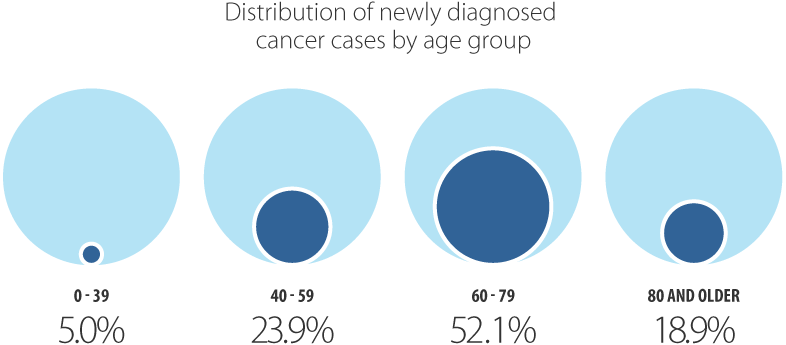
Ages 60 to 79 years
Of all new cases, 52.1% occurred in people 60 to 79 years of age.
This age group was more likely than other age groups to be diagnosed with the most common cancers:
- 46.0% of all new cases of breast cancer
- 51.1% of new cases of colorectal cancer
- 62.6% of new cases of lung cancer a
- 69.5% of new cases of prostate cancer
Ages 80 and older
Of all new cases, 18.9% occurred in people 80 years of age or older, with prostate and female breast being the leading cancers.
Cancer incidence increased with age, from a rate of 59.6 per 100,000 in people diagnosed at age 39 or younger to 2,559.7 per 100,000 in those diagnosed at age 80 or older. Rates varied by cancer type. Incidence rates for the following cancer types increased significantly with age:
- Malignant cancers of the brain and other nervous system
- Colon (including right-sided colon)
- Leukemia (including acute myeloid leukemia, acute monocytic leukemia and chronic myeloid leukemia)
- Lymphoma (including non-Hodgkin lymphoma and extranodal non-Hodgkin lymphoma)
- Melanoma of the skin
Testicular cancer and acute lymphocytic leukemia showed non-significant decreases with age, while all other cancer types increased non-significantly with age.
Incidence Trends by Cancer Type
From 1981 to 2000, the cancer incidence rate for all cancers combined increased by 0.5% per year, remained stable until 2011 and then decreased by 1.2% per year until 2016 (Table 5.5).
Among males, the incidence rate increased by 0.8% per year between 1981 and 1992, remained stable and then began decreasing in 2007 by 1.6% per year until 2016. Although the cancer incidence rate among females has not seen a similar decrease, the incidence rate has stabilized in recent years following a steady increase by 0.4% per year between 1981 and 2012.
Table 5.5 Annual percent change in age-standardized incidence rates by cancer type and sex, Ontario, 1981 to 2016
| Cancer type | Both sexes | |
|---|---|---|
| Period | APC (%) | |
| All cancers | 1981 - 2000 | 0.5* |
| 2000 - 2011 | -0.1 | |
| 2011 - 2016 | -1.2* | |
| Brain and other nervous system - malignant | 1981 - 2009 | -0.3* |
| 2009 - 2016 | -2* | |
| Glioblastoma | 1981 - 2001 | 2* |
| 2001 - 2005 | -4.5 | |
| 2005 - 2016 | 2.3* | |
| Meninges - malignant | 1981 - 1998 | 2.4* |
| 1998 - 2016 | -7.3* | |
| Brain and other nervous system - Non-malignant | n/a | ** |
| Meninges - non-malignant | n/a | ** |
| Pituitary, pineal and craniopharyngeal duct | n/a | ** |
| Breast (female) | n/a | n/a |
| Cervix | n/a | n/a |
| Ovary | n/a | n/a |
| Prostate | n/a | n/a |
| Testis | n/a | n/a |
| Uterus | n/a | n/a |
| Uterus - endometrial | n/a | n/a |
| Uterus - uterine sarcoma | n/a | n/a |
| Colorectal | 1981 - 1996 | -0.7* |
| 1996 - 2000 | 0.9 | |
| 2000 - 2008 | -0.9* | |
| 2008 - 2016 | -2.3* | |
| Colon excluding rectum | 1981 - 1985 | 1.2 |
| 1985 - 1995 | -1.1* | |
| 1995 - 2008 | -0.4* | |
| 2008 - 2016 | -2.4* | |
| Colon - left sided | 1981 - 2004 | -1* |
| 2004 - 2008 | 2 | |
| 2008 - 2012 | -5.6* | |
| 2012 - 2016 | -2 | |
| Colon - right sided | 1981 - 2010 | 0.1 |
| 2010 - 2016 | -2.4* | |
| Rectum and rectosigmoid junction | 1981 - 1997 | -0.6* |
| 1997 - 2001 | 3.7* | |
| 2001 - 2016 | -1.9* | |
| Rectosigmoid junction | 1981 - 1991 | 4.3* |
| 1991 - 1996 | -3.2 | |
| 1996 - 2000 | 9.5 | |
| 2000 - 2016 | -3.9* | |
| Rectum | 1981 - 1985 | 0.2 |
| 1985 - 1991 | -3.3* | |
| 1991 - 2008 | 0.4* | |
| 2008 - 2016 | -1.8* | |
| Esophagus | 1981 - 2007 | 0.1 |
| 2007 - 2011 | 3.3 | |
| 2011 - 2016 | -4.4* | |
| Esophagus - adenocarcinoma | 1981 - 1996 | 5* |
| 1996 - 2012 | 2.8* | |
| 2012 - 2016 | -2.8 | |
| Esophagus - squamous cell carcinoma | 1981 - 2016 | -2.2* |
| Liver | 1981 - 1999 | 4.9* |
| 1999 - 2007 | 2.6* | |
| 2007 - 2011 | 10.9* | |
| 2011 - 2016 | 0 | |
| Pancreas | 1981 - 2003 | -0.8* |
| 2003 - 2016 | 1.5* | |
| Stomach | 1981 - 1993 | -2.5* |
| 1993 - 2008 | -1.5* | |
| 2008 - 2012 | 2 | |
| 2012 - 2016 | -1.5 | |
| Larynx | 1981 - 1991 | -0.9 |
| 1991 - 2016 | -2.6* | |
| Oral cavity & pharynx | 1981 - 2004 | -1.8* |
| 2004 - 2012 | 2.3* | |
| 2012 - 2016 | -1.8 | |
| Hypopharynx | 1981 - 2016 | -2.4* |
| Lip and oral cavity | 1981 - 1990 | -1.1 |
| 1990 - 2003 | -3.7* | |
| 2003 - 2012 | 2.7* | |
| 2012 - 2016 | -3.8 | |
| Nasopharynx | 1981 - 2016 | -0.1 |
| Oropharynx | 1981 - 1998 | -0.6 |
| 1998 - 2016 | 2.4* | |
| Thyroid | 1981 - 1998 | 4.7* |
| 1998 - 2002 | 12.9* | |
| 2002 - 2012 | 6.8* | |
| 2012 - 2016 | -2 | |
| Thyroid - anaplastic | 1981 - 2016 | -0.6 |
| Thyroid - follicular | 1981 - 2016 | -0.9* |
| Thyroid - medullary | 1981 - 2016 | 2* |
| Thyroid - papillary | 1981 - 2012 | 9.1* |
| 2012 - 2016 | -2.9 | |
| Leukemia | 1981 - 2016 | 0.2* |
| Acute lymphocytic leukemia | 1981 - 2016 | 0.8* |
| Acute monocytic leukemia | 1981 - 2016 | 2.7* |
| Acute myeloid leukemia | 1981 - 2016 | 0.8* |
| Chronic lymphocytic leukemia | 1981 - 2000 | 0.3 |
| 2000 - 2004 | 6.3 | |
| 2004 - 2016 | -2.1* | |
| Chronic myeloid leukemia | 1981 - 2004 | -0.9* |
| 2004 - 2016 | 1.9* | |
| Lymphoma | 1981 - 1998 | 1.6* |
| 1998 - 2008 | 0.5 | |
| 2008 - 2016 | 2.6* | |
| Hodgkin lymphoma | 1981 - 2016 | -0.4* |
| Non-hodgkin lymphoma | 1981 - 1998 | 2* |
| 1998 - 2008 | 0.5 | |
| 2008 - 2012 | 4.1* | |
| 2012 - 2016 | 1.2 | |
| Non-hodgkin lymphoma - extranodal | 1981 - 2007 | 7.2* |
| 2007 - 2012 | 36.9* | |
| 2012 - 2016 | 0.3 | |
| Non-hodgkin lymphoma - nodal | 1981 - 1990 | 2.7* |
| 1990 - 2007 | 0.7* | |
| 2007 - 2011 | -8.8* | |
| 2011 - 2016 | -1.2 | |
| Myeloma | 1981 - 2004 | 0.7* |
| 2004 - 2008 | -3 | |
| 2008 - 2012 | 5.8* | |
| 2012 - 2016 | 1 | |
| Melanoma of the skin | 1981 - 1987 | 5.2* |
| 1987 - 1992 | -1.4 | |
| 1992 - 2016 | 2.2* | |
| Melanoma (non-cutaneous) | 1981 - 2016 | 0.5 |
| Melanoma - mucosal | 1981 - 2006 | -0.6 |
| 2006 - 2010 | 43.8 | |
| 2010 - 2016 | -4.8 | |
| Melanoma - ocular | 1981 - 2016 | -0.2 |
| Lung | 1981 - 1989 | 1.3* |
| 1989 - 2008 | -0.8* | |
| 2008 - 2012 | 0.8 | |
| 2012 - 2016 | -2.8* | |
| Lung - adenocarcinoma | 1981 - 1992 | 4.3* |
| 1992 - 2008 | -0.4 | |
| 2008 - 2012 | 8.6* | |
| 2012 - 2016 | 0.1 | |
| Lung - large cell | 1981 - 2000 | 0.6 |
| 2000 - 2004 | -15.5* | |
| 2004 - 2016 | -7.3* | |
| Lung - small cell | 1981 - 1988 | 7* |
| 1988 - 2011 | -0.4* | |
| 2011 - 2016 | -3.1* | |
| Lung - squamous cell | 1981 - 1988 | 0.3 |
| 1988 - 2008 | -3.5* | |
| 2008 - 2012 | 4.1 | |
| 2012 - 2016 | -2.3 | |
| Bladder‡ | 1989 - 2003 | -0.5 |
| 2003 - 2016 | -2.1* | |
| Kidney | 1981 - 1989 | 5.3* |
| 1989 - 1996 | -0.7 | |
| 1996 - 2016 | 1.7* | |
*Statistically significant trend
**Too few cases to calculate
†Bladder cancer trend begins at 1989 due to classification changes and excludes carcinomas in situ
Notes:
- IARC/IACR multiple primary rules used when presenting trends over time.
- Rates are standardized to the 2011 Canadian population.
- Only selected subsites and histological subtypes of major cancers are shown. As a result, counts for these may not sum to the total for the cancer type.
Analysis by: Surveillance, Analytics and Informatics, CCO
Data source: Ontario Cancer Registry (December 2018), CCO
| Cancer type | Males | |
|---|---|---|
| Period | APC (%) | |
| All cancers | 1981 - 1992 | 0.8* |
| 1992 - 2007 | -0.1 | |
| 2007 - 2016 | -1.6* | |
| Brain and other nervous system - malignant | 1981 - 2016 | -0.5* |
| Glioblastoma | 1981 - 2016 | 0.9* |
| Meninges – Malignant | 1981 - 1995 | 4.7* |
| 1995 - 2016 | -5.6* | |
| Brain and other nervous system - Non-malignant | n/a | ** |
| Meninges - non-malignant | n/a | ** |
| Pituitary, pineal and craniopharyngeal duct | n/a | ** |
| Breast (female) | n/a | n/a |
| Cervix | n/a | n/a |
| Ovary | n/a | n/a |
| Prostate | 1981 - 1993 | 4.9* |
| 1993 - 2007 | 1.2* | |
| 2007 - 2016 | -5.9* | |
| Testis | 1981 - 2016 | 1.3* |
| Uterus | n/a | n/a |
| Uterus - endometrial | n/a | n/a |
| Uterus - uterine sarcoma | n/a | n/a |
| Colorectal | 1981 - 2008 | -0.3* |
| 2008 - 2016 | -2.7* | |
| Colon excluding rectum | 1981 - 2008 | -0.4* |
| 2008 - 2016 | -2.4* | |
| Colon - left sided | 1981 - 2004 | -0.7* |
| 2004 - 2008 | 2.5 | |
| 2008 - 2012 | -6.1* | |
| 2012 - 2016 | -1.7 | |
| Colon - right sided | 1981 - 2010 | 0.2 |
| 2010 - 2016 | -2.2* | |
| Rectum and rectosigmoid junction | 1981 - 1997 | -0.3 |
| 1997 - 2001 | 3.5 | |
| 2001 - 2016 | -2* | |
| Rectosigmoid junction | 1981 - 2001 | 2.6* |
| 2001 - 2016 | -3.6* | |
| Rectum | 1981 - 1995 | -1.4* |
| 1995 - 2006 | 0.9* | |
| 2006 - 2016 | -2.1* | |
| Esophagus | 1981 - 2006 | 0.3 |
| 2006 - 2011 | 3.1 | |
| 2011 - 2016 | -4.8* | |
| Esophagus - adenocarcinoma | 1981 - 1991 | 6.8* |
| 1991 - 2012 | 3* | |
| 2012 - 2016 | -4.1 | |
| Esophagus - squamous cell carcinoma | 1981 - 2016 | -2.4* |
| Liver | 1981 - 2012 | 4.6* |
| 2012 - 2016 | 0.7 | |
| Pancreas | 1981 - 2004 | -1.3* |
| 2004 - 2016 | 2.2* | |
| Stomach | 1981 - 2008 | -1.9* |
| 2008 - 2016 | 0.5 | |
| Larynx | 1981 - 2016 | -2.3* |
| Oral cavity & pharynx | 1981 - 2006 | -2.1* |
| 2006 - 2012 | 4.2* | |
| 2012 - 2016 | -2.8 | |
| Hypopharynx | 1981 - 2016 | -2.3* |
| Lip and oral cavity | 1981 - 2005 | -3.6* |
| 2005 - 2012 | 3.5 | |
| 2012 - 2016 | -5.8 | |
| Nasopharynx | 1981 - 2016 | 0 |
| Oropharynx | 1981 - 1998 | -0.7 |
| 1998 - 2016 | 3* | |
| Thyroid | 1981 - 1997 | 4.1* |
| 1997 - 2012 | 7.7* | |
| 2012 - 2016 | 1.3 | |
| Thyroid - anaplastic | 1981 - 2016 | 2.1* |
| Thyroid - follicular | 1981 - 2016 | -0.9* |
| Thyroid - medullary | n/a | n/a |
| Thyroid - papillary | 1981 - 2012 | 8.5* |
| 2012 - 2016 | 2.2 | |
| Leukemia | 1981 - 2016 | 0.1 |
| Acute lymphocytic leukemia | 1981 - 2016 | 0.7* |
| Acute monocytic leukemia | 1981 - 2016 | 2.4* |
| Acute myeloid leukemia | 1981 - 2016 | 0.8* |
| Chronic lymphocytic leukemia | 1981 - 1999 | 0 |
| 1999 - 2003 | 6.9 | |
| 2003 - 2016 | -1.8* | |
| Chronic myeloid leukemia | 1981 - 1997 | 0.7 |
| 1997 - 2002 | -6 | |
| 2002 - 2016 | 2.1* | |
| Lymphoma | 1981 - 2009 | 1.2* |
| 2009 - 2016 | 2.8* | |
| Hodgkin lymphoma | 1981 - 2016 | -0.7* |
| Non-hodgkin lymphoma | 1981 - 2009 | 1.5* |
| 2009 - 2016 | 3* | |
| Non-hodgkin lymphoma - extranodal | 1981 - 2007 | 7.2* |
| 2007 - 2012 | 38.1* | |
| 2012 - 2016 | 0.1 | |
| Non-hodgkin lymphoma - nodal | 1981 - 2007 | 1.3* |
| 2007 - 2011 | -9.7* | |
| 2011 - 2016 | -0.1 | |
| Myeloma | 1981 - 2004 | 0.6* |
| 2004 - 2008 | -3.3 | |
| 2008 - 2012 | 7.2* | |
| 2012 - 2016 | 0.1 | |
| Melanoma of the skin | 1981 - 1988 | 5.7* |
| 1988 - 1992 | -1.4 | |
| 1992 - 2016 | 2.3* | |
| Melanoma (non-cutaneous) | 1981 - 2016 | 0.6* |
| Melanoma - mucosal | ** | ** |
| Melanoma - ocular | 1981 - 2016 | 0 |
| Lung | 1981 - 1989 | -0.1 |
| 1989 - 2008 | -2.1* | |
| 2008 - 2012 | 0.6 | |
| 2012 - 2016 | -4.2* | |
| Lung - adenocarcinoma | 1981 - 1992 | 3.1* |
| 1992 - 2008 | -1.5* | |
| 2008 - 2012 | 8.4* | |
| 2012 - 2016 | -1.2 | |
| Lung - large cell | 1981 - 2000 | -0.6 |
| 2000 - 2004 | -17.9* | |
| 2004 - 2016 | -6.8* | |
| Lung - small cell | 1981 - 1990 | 3.5* |
| 1990 - 2016 | -1.7* | |
| Lung - squamous cell | 1981 - 1988 | -0.6 |
| 1988 - 2008 | -4.4* | |
| 2008 - 2012 | 3.2 | |
| 2012 - 2016 | -2.5 | |
| Bladder‡ | 1989 - 2016 | -1.4* |
| Kidney | 1981 - 1989 | 4.6* |
| 1989 - 2001 | 0 | |
| 2001 - 2016 | 2.2* | |
*Statistically significant trend
**Too few cases to calculate
†Bladder cancer trend begins at 1989 due to classification changes and excludes carcinomas in situ
Notes:
- IARC/IACR multiple primary rules used when presenting trends over time.
- Rates are standardized to the 2011 Canadian population.
- Only selected subsites and histological subtypes of major cancers are shown. As a result, counts for these may not sum to the total for the cancer type.
Analysis by: Surveillance, Analytics and Informatics, CCO
Data source: Ontario Cancer Registry (December 2018), CCO
| Cancer type | Females | |
|---|---|---|
| Period | APC (%) | |
| All cancers | 1981 - 2012 | 0.4* |
| 2012 - 2016 | -0.4 | |
| Brain and other nervous system - malignant | 2000 - 2016 | -1.2* |
| Glioblastoma | 1981 - 2001 | 2* |
| 2001 - 2005 | -6.8 | |
| 2005 - 2016 | 3.5* | |
| Meninges - malignant | 1981 - 1999 | 1.4 |
| 1999 - 2016 | -8* | |
| Brain and other nervous system - Non-malignant | n/a | ** |
| Meninges - Non-malignant | n/a | n/a |
| Pituitary, pineal and craniopharyngeal duct | n/a | ** |
| Breast (female) | 1981 - 1992 | 2* |
| 1992 - 2016 | -0.2* | |
| Cervix | 1981 - 2004 | -2.1* |
| 2004 - 2016 | -0.9 | |
| Ovary | 1981 - 2002 | 0.3* |
| 2002 - 2016 | -1.2* | |
| Prostate | n/a | n/a |
| Testis | n/a | n/a |
| Uterus | 1981 - 1989 | -2.4* |
| 1989 - 2005 | 0.5* | |
| 2005 - 2011 | 4* | |
| 2011 - 2016 | 1 | |
| Uterus - endometrial | 1981 - 1990 | -2.6* |
| 1990 - 2005 | 0.7* | |
| 2005 - 2011 | 4.8* | |
| 2011 - 2016 | 1 | |
| Uterus - uterine sarcoma | 1981 - 2016 | 1* |
| Colorectal | 1981 - 1996 | -1.2* |
| 1996 - 2000 | 1.6 | |
| 2000 - 2016 | -1.7* | |
| Colon excluding rectum | 1981 - 2009 | -0.8* |
| 2009 - 2016 | -2.5* | |
| Colon - left sided | 1981 - 2009 | -1.3* |
| 2009 - 2016 | -3.3* | |
| Colon - right sided | 1981 - 2011 | -0.1 |
| 2011 - 2016 | -3.3* | |
| Rectum and rectosigmoid junction | 1981 - 1996 | -1.4* |
| 1996 - 2000 | 4.1 | |
| 2000 - 2016 | -1.6* | |
| Rectosigmoid junction | 1981 - 1991 | 4* |
| 1991 - 1996 | -5 | |
| 1996 - 2000 | 12 | |
| 2000 - 2016 | -4.3* | |
| Rectum | 1981 - 1991 | -3.1* |
| 1991 - 2016 | -0.1 | |
| Esophagus | 1981 - 2016 | -0.7* |
| Esophagus - adenocarcinoma | 1981 - 2016 | 3.1* |
| Esophagus - squamous cell carcinoma | 1981 - 2016 | -2* |
| Liver | 1981 - 2008 | 3.4* |
| 2008 - 2012 | 14.7* | |
| 2012 - 2016 | -3 | |
| Pancreas | 1981 - 2006 | -0.4* |
| 2006 - 2012 | 2.9* | |
| 2012 - 2016 | -2.1 | |
| Stomach | 1981 - 1998 | -2.9* |
| 1998 - 2016 | -0.1 | |
| Larynx | 1981 - 1988 | 3.2 |
| 1988 - 2016 | -2.9* | |
| Oral cavity & pharynx | 1981 - 2003 | -1* |
| 2003 - 2016 | 0.5 | |
| Hypopharynx | 1981 - 2016 | -3.2* |
| Lip and oral cavity | 1981 - 2003 | -1.1* |
| 2003 - 2016 | 1.4* | |
| Nasopharynx | 1981 - 2016 | -0.4 |
| Oropharynx | 1981 - 2016 | -0.1 |
| Thyroid | 1981 - 1998 | 4.9* |
| 1998 - 2002 | 14.5* | |
| 2002 - 2012 | 6.4* | |
| 2012 - 2016 | -3* | |
| Thyroid - anaplastic | 1981 - 2016 | -1.6* |
| Thyroid - follicular | 1981 - 2016 | -0.9* |
| Thyroid - medullary | 1981 - 2016 | 1.4* |
| Thyroid - papillary | 1981 - 1998 | 8* |
| 1998 - 2002 | 14.3* | |
| 2002 - 2012 | 8.1* | |
| 2012 - 2016 | -3.6* | |
| Leukemia | 1981 - 2016 | 0.1 |
| Acute lymphocytic leukemia | 1981 - 2016 | 0.8* |
| Acute monocytic leukemia | 1981 - 2016 | 2.7* |
| Acute myeloid leukemia | 1981 - 2016 | 0.6* |
| Chronic lymphocytic leukemia | 1981 - 2007 | 1.1* |
| 2007 - 2016 | -2.1 | |
| Chronic myeloid leukemia | 1981 - 2003 | -1.1* |
| 2003 - 2016 | 2* | |
| Lymphoma | 1981 - 1998 | 1.7* |
| 1998 - 2008 | 0.4 | |
| 2008 - 2016 | 2.1* | |
| Hodgkin lymphoma | 1981 - 2016 | -0.1 |
| Non-hodgkin lymphoma | 11981 - 1998 | 1.9* |
| 1998 - 2008 | 0.5 | |
| 2008 - 2016 | 2.3* | |
| Non-hodgkin lymphoma - extranodal | 1981 - 2007 | 6.7* |
| 2007 - 2011 | 42.7* | |
| 2011 - 2016 | 4.1 | |
| Non-hodgkin lymphoma - nodal | 1981 - 1998 | 1.8* |
| 1998 - 2008 | -0.5 | |
| 2008 - 2012 | -9* | |
| 2012 - 2016 | -0.7 | |
| Myeloma | 1981 - 2001 | 0.8* |
| 2001 - 2008 | -1.4 | |
| 2008 - 2016 | 3* | |
| Melanoma of the skin | 1981 - 1987 | 4.1* |
| 1987 - 1992 | -2.4 | |
| 1992 - 2016 | 2* | |
| Melanoma (non-cutaneous) | 1981 - 2007 | -0.5 |
| 2007 - 2016 | 4 | |
| Melanoma - mucosal | ** | ** |
| Lung | 1981 - 1985 | 6.5* |
| 1985 - 1998 | 1.9* | |
| 1998 - 2012 | 0.5* | |
| 2012 - 2016 | -0.8 | |
| Lung - adenocarcinoma | 1981 - 1992 | 5.8* |
| 1992 - 2008 | 0.7* | |
| 2008 - 2012 | 8.7* | |
| 2012 - 2016 | 1.2 | |
| Lung - large cell | 1981 - 1999 | 3* |
| 1999 - 2016 | -9* | |
| Lung - small cell | 1987 - 1997 | 2.4* |
| 1997 - 2016 | -0.4 | |
| Lung - squamous cell | 1981 - 1995 | 1.5* |
| 1995 - 2007 | -2.6* | |
| 2007 - 2012 | 4.8* | |
| 2012 - 2016 | -1.9 | |
| Bladder‡ | 1989 - 2003 | -0.5 |
| 2003 - 2016 | -2.8* | |
| Kidney | 1981 - 1986 | 9.1* |
| 1986 - 2016 | 1.1* | |
*Statistically significant trend
**Too few cases to calculate
†Bladder cancer trend begins at 1989 due to classification changes and excludes carcinomas in situ
Notes:
- IARC/IACR multiple primary rules used when presenting trends over time.
- Rates are standardized to the 2011 Canadian population.
- Only selected subsites and histological subtypes of major cancers are shown. As a result, counts for these may not sum to the total for the cancer type.
Analysis by: Surveillance, Analytics and Informatics, CCO
Data source: Ontario Cancer Registry (December 2018), CCO
Recent incidence trends for the 4 most common cancers
Breast cancer
Since 1992, the age-standardized incidence rate (ASIR) for female breast cancer in Ontario has been steadily decreasing at 0.2% per year, likely due to the diminishing number of women with undetected cancer. Such a rise and fall in the incidence rate is characteristic of the introduction in a population of a new method of early diagnosis.
In addition, the use of hormone replacement therapy (HRT), associated with an increased risk of breast cancer among post-menopausal women, began to decline in Canada in the early 2000s.[25,26] This may also have contributed to a continuing decline in the breast cancer incidence rate in subsequent years.
Colorectal cancer
The ASIR for colorectal cancer among males declined by 2.7% per year from 2008 to 2016. Individually, incidence rates for both colon and rectal cancers in males also declined during this period.
Among females, the colorectal cancer incidence rate was stable between 1996 and 2000, and then decreased after 2000 at a rate of 1.7% per year. These trends may reflect the following opposing trends for colorectal cancer sub-sites:
- An increase in cancer of the rectosigmoid junction between 1996 and 2000
- An overall decrease in colon cancer between 1981 and 2016 in females
Lung cancer
In males, the ASIR for lung cancer was stable from 2008 to 2012 and has since declined by 4.2% per year. The incidence rate among females increased from the early 1980s until 2012 – although the upward trend slowed after 1995. Since 2012, the female rate has been stable.
The decline in the lung cancer incidence rate in males and the slow plateauing in the incidence rate in females over the last 2 decades reflects differences in historical smoking rates between the sexes.[27] While tobacco use is the primary cause of lung cancer, other causes include exposure to radon, asbestos, environmental tobacco smoke and air pollution.
The increasing trend of lung adenocarcinoma among females has also been seen in other jurisdictions.[28-30] One explanation for this trend may be the longer latency of the effect of smoking cessation on adenocarcinoma rates. Once a person quits smoking, their risks for other lung cancer subtypes decline faster than their risk for adenocarcinomas.[29]
Given the historical differences in smoking rates between males and females, the increasing rate of adenocarcinomas among females may reflect the delay between quitting smoking and lowering adenocarcinoma risk in women. Finally, the declining trend in the male rate has allowed the female rate to surpass it.
Prostate cancer
The ASIR for prostate cancer increased 1.2% per year from 1993 to 2007, and then fell by 5.9% per year between 2007 and 2016. An abrupt rise and fall in the incidence rate is common when a new method of early diagnosis is introduced, such as prostate-specific antigen (PSA) testing for prostate cancer. The decrease starting in 2011 may also reflect the effect of recommendations from the U.S. Preventive Services Task Force against using PSA testing for the routine screening of healthy males.[31]
Notable changes in trend for other cancers
Liver cancer
Incidence rates for liver cancer increased steeply between 1981 and 2011, although the rates have stabilized in recent years. Among males, the ASIR increased at a rate of 4.6% per year from 1981 to 2012 and has been stable since then. The trend was more pronounced among females, with the ASIR increasing by 3.4% per year from 1981 to 2008, by 14.7% per year from 2008 to 2012 and stabilizing in the most recent period.
A rising incidence rate of liver cancer may be the result of:
- increasing immigration from countries where certain risk factors (e.g., hepatitis B and C infections, exposure to aflatoxins) are more common[32]
- a higher prevalence of hepatitis C infection caused by needle sharing[33]
- increasing prevalence of obesity and diabetes[33]
Myeloma
The ASIR for myeloma increased by 5.8% per year between 2008 and 2012 before stabilizing in recent years. The increase was driven mainly by the increased rate in males, which went up by 7.2% per year between 2008 and 2012. The rate for females has been increasing by 3.0% per year since 2008.
Increasing trends in other jurisdictions suggest the rise in myeloma rates may be due to improvements in diagnostics and better registration of cases. [34]
Thyroid cancer
The ASIR for thyroid cancer increased significantly during the 1981 to 2016 period. The greatest increase occurred between 1998 and 2002, at 12.9% per year. This was mainly because of the increase in the female rate of 14.5% per year. The overall incidence rate continued to increase between 2002 and 2012, but at a slower pace of 6.8% per year, before stabilizing in recent years. Among females, the ASIR decreased by 3.0% per year starting in 2012.
The rising incidence rate has been attributed to the greater use of ultrasound and fine-needle aspiration, which may have improved the detection of subclinical tumours (i.e., early tumours that do not cause symptoms).[35-38] A similar change in trend among females has been seen in other jurisdictions,[39] which have reported that thyroid incidence rates among females have stabilized in recent years.
Uterine cancer
Following a period of declining incidence rates, the ASIR for uterine cancer increased by 4.0% per year from 2005 to 2011 before stabilizing in recent years. The increase was mainly because of increasing incidence rates for endometrial cancer over the same period (4.8% per year between 2005 and 2011).
Increasing incidence of endometrial cancer in other jurisdictions suggests trends may be linked to increasing rates of obesity and hormone therapy use as well as decreasing rates of pregnancy. All of these increase exposure to estrogen, a key risk factor for endometrial cancer.[40]
Thirty-Five Year Trend in Incidence
The age-standardized incidence rates (ASIR) from 1981 to 2016 for selected cancers are shown in Figure 5.3. These cancers represent the 4 most common cancers in Ontario (breast, prostate, lung and colorectal) as well as those with significantly increasing recent trends in ASIR.
Over the last 35 years (1981 to 2016) the average annual percent change (AAPC) in ASIR for males (Figure 5.4):
- increased most for thyroid (5.3%) and liver (4.2%) cancers, melanoma (2.6%), and kidney cancer (2.0%)
- remained stable for esophageal, pancreatic, and prostate cancers, leukemia, myeloma and all cancers combined
- decreased most for laryngeal (2.3%), lung (1.6%), bladder (1.4%) and stomach (1.4%) cancers
For females, the AAPC:
- increased most for thyroid (5.5%), liver (3.9%) and kidney (2.2%) cancers, and melanoma (1.7%)
- remained stable for pancreatic cancer, Hodgkin lymphoma and leukemia
- decreased most for laryngeal (1.7%), cervical (1.7%), bladder (1.6%) and stomach (1.5%) cancers
Incidence Trends by Age
Over the past 35 years, cancer incidence rates have been increasing among younger and middle-aged people, and decreasing among the elderly.
Ages 0 to 39
Among people under the age of 40, the cancer incidence rate increased by 0.5% per year between 1981 and 2001, then by 1.5% per year between 2001 and 2011 before stabilizing in recent years (Figure 5.5).
Different trends were seen in males and females. Among males, the rate increased by 1.8% per year between 1981 and 1991, remained stable until 2001 and has been increasing by 1.1% per year since. For females, the rate increased by 0.3% per year between 1981 and 1996, increased by 1.8% per year between 1996 and 2009, and has been stable since then. The increase in incidence among males is probably due to the increasing rates of testicular and thyroid cancers, and non-Hodgkin lymphoma in this age group (data not shown).
Among children ages 0 to 14 years, the average annual percent change (AAPC) in age-standardized incidence rates (ASIR) increased by 0.8% over the period from 1986 to 2016 and has been increasing by 1.7% per year between 2002 to 2016 (see Spotlight: Childhood Cancer Incidence Trend, Figure 5.S1).
For details about childhood cancer incidence trends, visit the POGO Surveillance Report.
Spotlight: Childhood Cancer Incidence Trend
Ages 40 to 59
Among people ages 40 to 59, the rate of cancer increased by 0.5% per year from 1981 to 2007 and then decreased by 0.5% per year from 2007 onward. While the trend among males was the same, the female rate has been increasing by 0.4% per year since 1981.
Ages 60 to 79
For those ages 60 to 79, the rate increased by 1.2% per year between 1981 and 1992, remained stable between 1992 and 2007, and has since been decreasing by 1.3% per year. The rate among males was similar, although the rate of decrease in the most recent period (2007 to 2016) has been greater, at 2.3% per year. Females in this age group had no decrease in incidence rate; their rate increased by 1.0% per year between 1981 and 1991, and then by 0.3% per year between 1991 and 2012 before stabilizing in the most recent period.
Ages 80 and older
In the oldest age group (those 80 and older), the incidence rate declined steadily throughout the whole period by 0.1% per year. While the male rate had 2 periods of decline, by 1.1% per year between 1991 and 2007 and 1.9% per year from 2011 onward, the female rate has been increasing slowly by 0.1% per year since 1981.
Incidence by Stage
“Cancer staging” refers to classifying people with cancer into groups according to the extent of the disease. “Stage at diagnosis” is the extent of the disease at the time of initial diagnosis.
A stage group (i.e., stage 0, 1, 2, 3 or 4) is based on distinct characteristics of a tumour that describe the extent of spread of a cancer in the body. Knowing the stage of the disease helps physicians plan appropriate treatment and determine the likely outcome or course of the disease. Information about stage at diagnosis is one of the most important factors for predicting the outcome for a person with cancer.
A cancer diagnosed at an early stage is more likely to be treated successfully. If the cancer has spread, treatment becomes more difficult and a person’s chances of survival are generally much lower.
The stage group is useful as a comparator within and across different cancer types, as well as for comparing trends over time. High-quality stage information at the population level supports healthcare providers, administrators, researchers and decision-makers in planning, evaluating and enhancing quality of care to improve treatment outcomes.
Population-level stage-at-diagnosis data with high completeness are available in Ontario for 5 cancers: female breast, prostate, colorectal, lung and cervical (see Data Source for important notes about this data).
The majority of breast, prostate and cervical cancer cases, and half of all staged colorectal cancer cases were diagnosed at stage 1 or 2 (Figure 5.6). This may partly be because screening is available for breast, colorectal and cervical cancers, which increases the likelihood of finding these cancers at early stages. The distribution of stage varied by cancer type:
- The majority of staged breast cancer cases were diagnosed at stage 1 (44.7%) or stage 2 (37.7%) in 2016.
- Cervical cancer was even more likely to be diagnosed at stage 1 (55.1%) than breast cancer. Females diagnosed at a later stage are less likely to have been routinely screened.[41] Despite the successes of screening programs in reducing cervical cancer new cases and deaths, 10.1% of cases were still not diagnosed until stage 4.
- The majority of staged colorectal cancer cases were diagnosed at stage 2 (26.0%) or stage 3 (31.5%). The distribution of stage was similar for the colorectal cancer sub-sites; however, a greater proportion of cancers of the rectum (35.7%) and rectosigmoid junction (36.5%) were diagnosed at stage 3.
- Prostate cancer cases were most likely to be diagnosed at stage 2 (51.3%) followed by stage 1 (22.5%).
- Lung cancer cases were the most likely to be diagnosed at stage 4, which accounted for 46.3% of all staged lung cancer cases. Out of all lung cancer subtypes, small cell lung cancer had the greatest proportion (68.1%) of cases diagnosed at stage 4.
The majority of breast, prostate and cervical cancer cases, and half of all staged colorectal cancer cases were diagnosed at stage 1 or 2.
Incidence by stage among screening-program-eligible cases
Among people within the screening-eligible age groups for Ontario’s population-based breast, cervical and colorectal screening programs, a greater proportion of cases was diagnosed at stage 1 (Figure 5.7) compared with all ages (Figure 5.6):
- 51% of breast cancer cases diagnosed at stage 1 among females ages 50 to 74 (Ontario Breast Screening Program eligible age group) compared with 45% among females of all ages
- 58% of cervical cancer cases diagnosed at stage 1 among females ages 21 to 69 (Ontario Cervical Screening Program eligible age group) compared with 55% among females of all ages
- 26% of colorectal cancer cases diagnosed at stage 1 among people ages 50 to 74 (ColonCancerCheck eligible age group) compared with 24% among people of all ages.
Reasons for the lower proportion of stage 1 colorectal cancers may include lower screening participation rates (compared with breast and cervical screening) and inappropriate screening of people with symptoms. For colorectal cancer, a decrease in stage 4 diagnoses is more important than an increase in stage 1, because cancers at stages 1 to 3 have a fairly good prognosis compared with those at stage 4. However, not all cancers diagnosed within the screening age groups are screening-detected cancers.
Trend in stage distribution
The distribution of stage at diagnosis for female breast, prostate, colorectal, lung and cervical cancers has changed over the 2010 to 2016 period (Figure 5.8).
- The proportion of prostate cancer cases diagnosed at stage 1 has decreased from 27% in 2010 to 22% in 2016. On the other hand, the proportion of cases diagnosed at stage 4 has increased from 8% in 2010 to 13% in 2016. This shift in distribution by stage may be partly because less opportunistic screening for prostate cancer took place following a recommendation against screening using PSA.[31,42] This would have resulted in the detection of fewer early stage cases and, likely, of more symptomatic cases at later stages.
- The proportion of lung cancer cases diagnosed at stage 1 has increased from 18% in 2010 to 26% in 2016, while the proportion of cases diagnosed at stage 4 has decreased from 57% in 2010 to 46% in 2016. Some evidence suggests that this downward shift in stage at diagnosis may reflect earlier detection resulting from recent lung cancer awareness campaigns.[43]
- The stage distribution has remained relatively unchanged for colorectal cancers. There was no change in the proportion of cases diagnosed at early stages over the 2010 to 2016 period. The proportion of cases diagnosed at later stages shifted slightly from 20% diagnosed at stage 4 in 2010 to 18% in 2016, and from 30% diagnosed at stage 3 in 2010 to 32% in 2016.
- The proportion of cervical cancer cases diagnosed at stage 1 dropped from 62% in 2010 to 55% in 2016, while the proportion of cases diagnosed at stage 2 increased from 9% in 2010 to 21% in 2016. However, the overall proportion of early stage cases (stages 1 and 2) increased from 71% to 76%.
- The stage distribution of breast cancer cases remained relatively stable, with the proportion of early stage cases increasing slightly (from 43% to 45% for stage 1 cases and 37% to 38% for stage 2) over the 2010 to 2016 period.
